- Increased neck pain;
- Heaviness in the back of the head;
- There is a slight tingling sensation in the hands.
important! Remember that the disease develops slowly and in the first stages it is much easier to control the progress of the destructive process than to treat the later stages!
who is in danger
How the disease develops
- The first stage is characterized by an almost complete absence of symptoms. The disease can only be diagnosed through routine tests. Mild pain may sometimes occur, which many people consider to be a sign of stress or fatigue. In the first stage, the nucleus pulposus is destroyed, so the vertebrae begin to bear more severe loads. As a result, a degenerative dystrophic process occurs. Initial symptoms include: mild headache that disappears quickly, "inner neck" spasm syndrome, and noticeable muscle tension in the upper back.
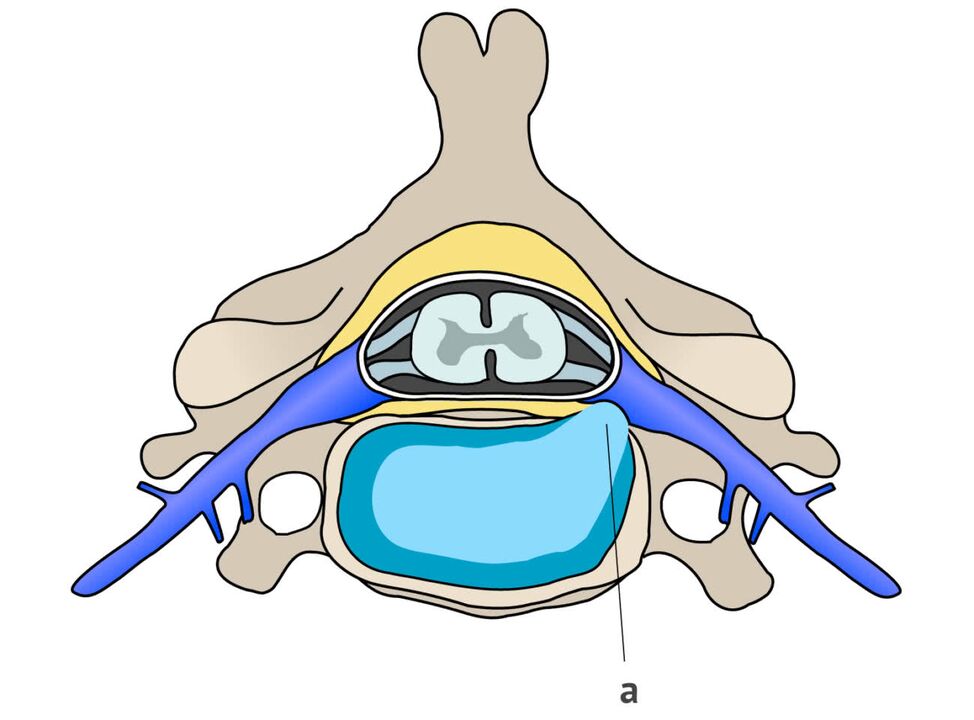
- In the second stage of the disease, cracks develop on the sides of the disc due to pressure. They are not very deep yet, but already help to squeeze out the nucleus. During diagnosis, herniation and reduced disc height are often discovered. This stage is characterized by frequent and persistent pain. A person loses strength, becomes numb in certain areas of the face, and stiffens movements due to fear of new painful sensations.
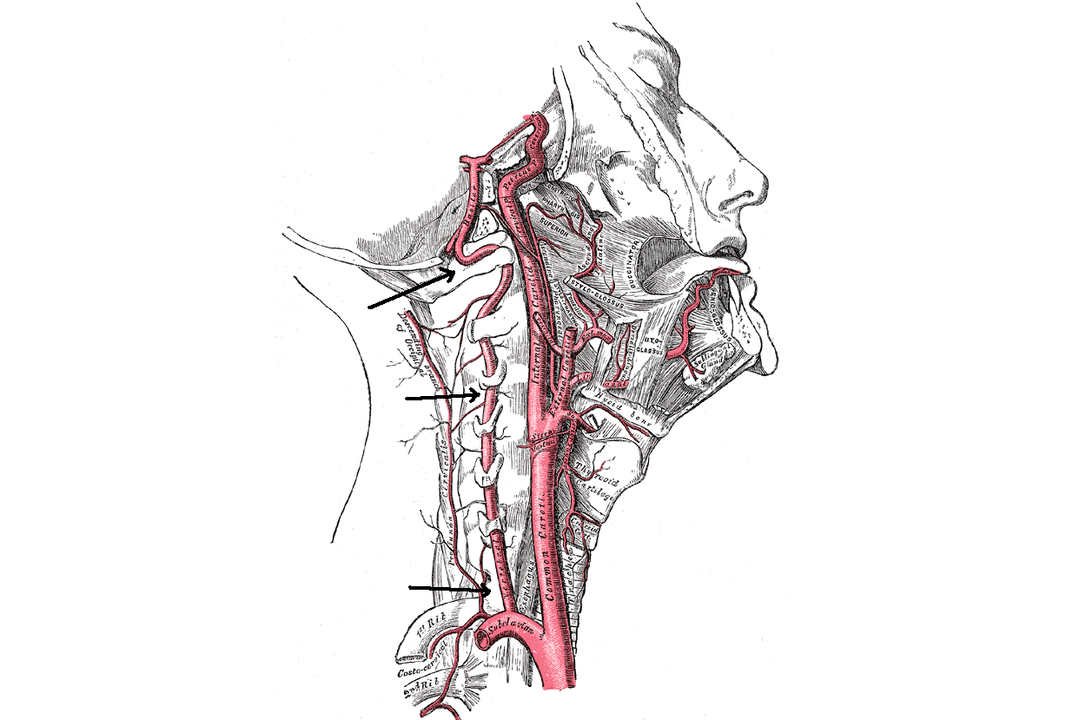
- The third stage is characterized by the formation of a hernia in the neck area between the vertebrae. All tissues and blood vessels located in the area - veins, muscles, nerves, arteries - are also affected. The pain spreads smoothly from the neck to the occiput area. Particularly sensitive when moving the head. The patient also began complaining of dizziness due to insufficient blood flow in the vertebral artery.
- In stage four, osteophytes form - the width of the bone tissue increases because the body and brain are literally signaling that more area is needed to distribute the load. As a result, the nerves of the vertebrae are compressed, the spaces between the vertebrae are reduced, severe stiffness occurs, and sometimes even the inability to move. All adjacent joints are damaged. At this stage, to eliminate the cause and "contain" cervical osteochondrosis, long-term and difficult treatment is required, including surgical intervention.
Symptoms and characteristics of cervical osteochondrosis
important! Pressure on blood vessels and nerves can cause discomfort and severe pain.
- The first group is characterized by neuropathological manifestations due to the influence of inflammatory processes and changes in the tissues of peripheral parts of the nervous system;
- The second group relates to the effects of the procedure on the spinal cord;
- The third group includes signs that rely on disruption of nerve ending processes leading to the brain.
- feeling weak;
- Numbness in one or more fingers;
- Most of the hand will then become numb.
- cough;
- stomachache;
- Liver discomfort;
- Lung pain.
Headaches caused by cervical osteochondrosis are of little help with the use of traditional pain relievers.
- increase stimulation;
- Sensitive and intermittent sleep;
- Fatigues quickly.
syndrome
Humeral periscapulitis
- continuous;
- pain;
- pain.
radiculopathy syndrome
- Pain is observed in the forearm, shoulder blade area and moves to the front of the chest;
- It becomes difficult to move your neck and you feel pain and stiffness;
- The skin on the hands becomes less sensitive, becomes numb, and feels like "goosebumps";
- A person cannot raise their hands from one side of the affected area.
irritant reflex syndrome
cardiac syndrome
vertebral artery syndrome
- headaches of varying degrees;
- Vestibular organ disorder (staggering, loss of balance);
- mild and severe dizziness;
- feel sick and vomit;
- Throat and eye symptoms (reduced vision, veiling in front of eyes).
With vertebral artery syndrome, burning pain may occur not only in the neck but also in the back of the head. A feeling of lethargy, resentment, and irritability develops. Anxiety levels increase, and sleep and memory may be disrupted.



















