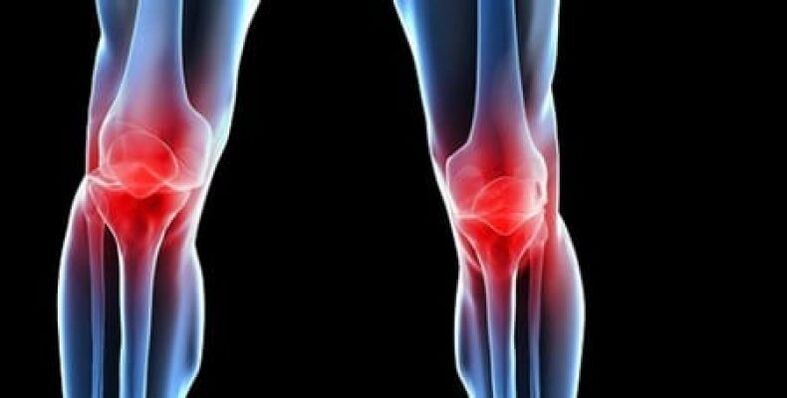
One of the most common complaints doctors hear from patients is knee pain. The cause of this pain isn't always immediately obvious. The knee can be affected by various conditions, such as arthropathy of the knee joint. It is also called arthropathy.
Knee arthropathy is a non-inflammatory joint injury that often results in cartilage destruction, skeletal deformities, and limited mobility. This disease has the code M17 in the International Classification of Diseases (ICD-10).

All patients can be divided into two groups. The first group included young adults, more commonly young men, with damage to one knee and less commonly both knees. They have injuries or knee surgery in their medical history.
The second group consisted of obese, middle-aged or elderly people, and more commonly women, who developed knee joint disease in multiple parts of the body at the same time.
Symptoms of knee osteoarthritis
Symptoms of knee osteoarthritis gradually worsen. Patients may not know they are sick for years until they notice significant knee deformity or severe pain.
At the same time, knee arthritis in the early stage of the disease is most often accompanied by a feeling of knee discomfort and pain, and few people seek medical attention.
Women who are prone to obesity, especially those after the age of 40, are more likely to develop the disease.
Varicose veins also contribute to the development of the disease. At this stage, the disease can be treated at home without the use of tablets and ointments.
The pain is not sudden, it comes on gradually and lasts for years. They usually occur during exercise, walking, and other physical activities.
Acute pain may not be a symptom of arthropathy, but the result of a crack, meniscus injury, or bruising. Severe pain becomes a motivation to seek a specialist.
Pain usually gets worse when:
- while walking;
- standing for long periods of time;
- during slopes;
- when lifting the body from a sitting position;
- When carrying heavy objects.
During these movements, the greatest load is placed on the joint, so if a patient experiences severe discomfort, a diagnosis of stage II knee arthritis can already be made. A person tries to move less, adopting a still position to avoid pain, but with continued physical activity, the discomfort reappears.
Deformative osteoarthritis of the knee is accompanied by symptoms such as deformity. It has become evident in the second or third stage of the disease. Her first sign: her knee was slightly swollen, but remained in place. In later stages, the shape of the knee changes, making one leg shorter or longer.
One of the most typical symptoms is joint tightening, which is evident in the second and third stages. The most important thing is to distinguish between the loud crunching sound of a healthy person's joints and the deaf, dry crunching sound of a patient. This sound can lead to weakened ligamentous organs or high joint mobility.
In order to ensure the immobility of the knee joint, it is recommended to wear knee pads.
form of knee joint disease
There are two forms of the disease:
- Primary: Occurs due to congenital abnormalities in joint development.
- Minor: Occurs due to illness and injury.
The predominant form of knee osteoarthritis usually develops in childhood and is caused by improperly formed ligaments and joints. They are heavily loaded and deformed during physical activity.
Secondary forms of this disease are caused by:
- Injuries (bruises, sprains, displacements, fractures) that result in the destruction of bone, ligament, and cartilage structures. All of these are post-traumatic forms of the disease.
- Surgery when the meniscus is displaced can destroy the structural integrity of the knee joint.
- Excessive load on the legs (typical of weightlifters).
- obesity. Being overweight puts pressure on the cartilage in the knee joint.
- passive lifestyle.
- diabetes.
- age.
- Arthritis (a joint inflammatory process). Long-term disease is accompanied by the formation of excess fluid in the joint cavity and leads to complications.
- Metabolic disturbances lead to salt deposition.
- Knee transplant.
- A condition that causes prolonged muscle spasms or vasospasm in the legs.
The development of the disease can take unilateral or bilateral forms. Trauma often causes left or right joint disease, and obesity is bilateral.
stage of disease
Knee disease is divided into three stages:
- It can take months or even years from the onset of the first stage to the obvious manifestation of the disease. The person complained of intermittent pain in the legs, especially when going up and down stairs and getting up in the morning. Pictures often show narrowing of the connections between the joints, and often patients don't see a doctor, but use traditional medicines -- ointments and tinctures.
- The second stage is characterized by more severe pain that does not stop with the immobility of the limb. A creaking sound occurs. Fluid builds up in the joint cavity, and X-rays show the deformation and growth of the bone. During this stage, the patient will do everything possible not to move the affected limb. The attending physician prescribes injections and chondroprotectants—drugs that help restore cartilage tissue.
- In the final third stage, the pain becomes persistent and often worsens with changing weather conditions. The X-ray showed a significant deformity of the knee joint, which could only be corrected by surgery, and the patient had to take a composite chondroprotective agent. The patient's gait changes: he walks with half-bent legs or rolls from side to side.
cause of disease. high-risk groups
overweight
In most cases, osteoarthritis deformans affects older adults. In a special risk group, women who are overweight after age 40. Obese people are 4 times more likely to develop pathology than normal-weight people. The pattern is simple: the heavier a person is, the faster and more severe the disease progresses. In this case, the form of the disease can be called acquired. It is the joints of the lower extremities that take the hit, as they are forced to take the greatest load.
Overweight people also face hormonal imbalances and metabolic disturbances, which can lead to the development of obesity and joint disease.
age
Seniors can be referred to as those who have reached the age of 60-65. In this population, 65-85% have osteoarthritis.
The reason is that age-related changes can negatively affect joint structure. Even ordinary walking can become a significant load and stimulate the development of disease, and the worn cartilage can no longer recover on its own.
Congenital diseases and genetic factors
The disease can affect young adults and those who are not overweight. Usually, in this case, the disease occurs due to a birth defect of the knee joint, for example, a lack of intra-articular lubrication. Genetics also plays an important role.
However, most patients with knee pain are persons of considerable age. Arthropathy is rare in young adults. Unfortunately, younger patients do not always receive the necessary treatment because not all physicians feel the need to give them the necessary attention.
high load
People who rely on manual labor for a living and athletes of all levels are also at risk for knee osteoarthritis. In this case, the disease becomes an occupational disease.
Surgery, Injury, and Other Illnesses
Surgery, trauma, and various diseases of the joints can cause arthropathy.

Knee osteoarthritis is often referred to as idiopathic when the cause remains unknown.
Diagnosis of knee joint disease
The diagnosis is made based on the patient's complaint, examination data, palpation of the diseased joint, and X-ray examination.
X-rays are a standard research method that allows you to confirm the diagnosis, determine the extent of pathological changes, monitor the dynamics of the process, and also rule out other pathological processes (such as tumors) in the tibia and femur.
It should be noted that major changes in knee joint structure on radiographs may not be present. Subsequently, the narrowing of the joint space and the compaction of the subchondral area are determined. The articular end of the femur, especially the tibia, is dilated, and the edges of the condyles are sharpened.
Auxiliary diagnostic methods are CT (computed tomography) and MRI (magnetic resonance imaging), which can study pathological changes in bone structure in more detail and identify changes in soft tissue.
How to Treat Knee Arthropathy
The more severe the stage of the disease, the more complex the treatment of arthropathy. The chronic nature of the pathology may remain in remission when active manifestations of the disease are minimized or completely absent.

Physiotherapy combined with chondroprotective drugs produces positive results.
Treatment options include:
- drug therapy (chondroprotective agents);
- operation treatment;
- Rehabilitation courses (kinesiology, massage, etc. ).
medical treatement
With drug therapy, the use of non-steroidal analgesics is prescribed. These medicines help relieve the pain and symptoms of synovitis (inflammation). Corticosteroids may be used if the pain is particularly severe or if the synovium of the knee is severely inflamed. These drugs are more powerful analgesic and anti-inflammatory than non-hormonal pain relievers. Muscle relaxants and antispasmodics will help the muscles around the joints get rid of spasms.
Antioxidants and vasodilators improve cartilage nutrition. The main drugs for conservative treatment of the disease are chondroprotective agents containing chondroitin and glucosamine sulfate (natural components of cartilage).
The use of causative drugs should be systemic and long-term.
physiotherapy
Physical therapy methods (UHF, ultrasound or light therapy) are considered additional means to speed up the healing process.
They also include:
- acupuncture. This approach relieves muscle spasms near the affected joints, normalizes their metabolic processes, and restores damaged cartilage tissue.
- Leech therapy. Leech treatment has the same effect as injections because it improves blood circulation.
- Laser therapy. Such procedures reduce inflammation, swelling, improve metabolism and neutralize pain.
- cryotherapy. Both liquid nitrogen and regular ice treatments work at home.
- Magnetic therapy. The effects of the magnetic field not only improve blood circulation in the tissue, but also reduce swelling and inflammation.
- Myoelectric stimulation. With the help of electrical micro-discharges of different frequencies, the muscles are recovered and strengthened, and the blood circulation of the extremities is improved.
Knee joint disease is effective with physical therapy because it reduces pain. The attending physician usually prescribes such treatments depending on the stage of the disease.
physiotherapy
Exercise therapy for knee osteoarthritis is one of the main means of restoring wasted muscle and must be done very carefully and slowly. If the patient feels that the pain is returning, they should stop exercising.

During therapeutic exercises, it is necessary to wear special knee braces. Rehabilitation sessions also include the use of these orthopedic devices, the goal of which is to reduce the load from the affected knee to the cane or prosthesis. Knee patients are often required to wear knee braces to reduce pain when walking.
Therapeutic gymnastics for arthropathy reduces the load on damaged joints and develops leg muscles. Exercises that put a load on the joints are strictly prohibited. Aqua gymnastics and swimming are ideal activities.
Orthopedic treatment
To reduce the load on the affected joints, the patient should use crutches. A good helper for knee osteoarthritis is an orthopedic shoe that provides a natural foot position and even load distribution.
massage
Massage relieves muscle spasms, reduces pain, and increases range of motion. The process also improves blood circulation and provides nutrients to the joints.
operation treatment
Significant decline in work capacity (especially up to age 45) requires surgery. The choice between corrective (removal of osteophytes) and radical (knee replacement) treatments depends on the stage of the disease, the patient's age, symptoms, and other factors.
Nutrition
As for special diets for arthropathy, it is usually to reduce the patient's weight, as being overweight can lead to overloading of the joints. It is recommended to eat small meals every 3 hours, eat lean meat (chicken, turkey, rabbit), exclude fat, and get the necessary protein from beans.
Refined oils should be replaced with unrefined oils, and salt intake should be limited. A therapeutic diet also means refusing canned, fried and smoked foods. To restore damaged cartilage, it is necessary to provide the body with carbohydrates, which are found in grains and whole-wheat flour.
In addition, it is recommended to drink more freshly squeezed juices, such as carrots, beets, apples, etc. , which can remove toxins from the body and reduce inflammation in the body.
Fish and various jellies act as chondroprotectants, helping to restore cartilage not only in the initial stages, but also during deterioration.
folk remedies
There are many ointments, compresses, and tinctures that are used by fans of traditional medicine. These medicines are usually made from herbal, medicinal bile, and they help improve circulation in the joints.
Compressions and ointments also relax the muscles, they are very effective, but they are practically useless in stage III arthropathy without the use of drugs.
Traditional medicine should not be ignored as they help relieve discomfort and reduce many symptoms of the disease. But in any case, you should consult your doctor and do not self-medicate.
There are contraindications, it is necessary to consult a specialist.
prevention
It is recommended to adhere to the following principles of a healthy lifestyle:
- Balanced diet;
- Quit bad habits (smoking, alcohol);
- sporty;
- maintain a healthy weight;
- Prevention of sports injuries (bruises, displacements, fractures).
There are several treatment options for knee osteoarthritis, depending on the patient's age and medical condition. Early prevention and control of the disease requires both exercise and timely treatment.



















